Did you know that more than one in five high school students in the United States reported using e-cigarettes in just the last 30 days? That startling statistic signals an urgent warning about teen vaping risks and their lasting consequences on young people’s health. As a parent, understanding what’s truly at stake—and how to protect your child—has never been more important.
Startling Statistics: The Alarming Rise of Teen Vaping Risks
"More than one in five high school students reported vaping in the last month, raising serious concerns about teen vaping risks and the long-term health effects on young people." – CDC Report
The numbers don’t lie—teen vaping risks are at an all-time high. In recent years, studies show a dramatic increase in e-cigarette use among both middle and high school students. According to the CDC, over 27% of high school students have tried vaping, a figure that’s more than doubled over the past five years. Worryingly, many of these young people believe vaping is safer than traditional tobacco products, despite mounting evidence of potential harm. This misconception, fueled by flavored vapes and slick marketing, makes it harder for parents to communicate the true dangers to their children. The proliferation of electronic cigarette devices on school campuses has now become a public health risk, with experts comparing its impact to the tobacco epidemic of decades past.
As electronic cigarette use surges among youth, public health authorities such as the American Lung Association and government organizations stress that these products deliver not only nicotine addiction but a host of unknown toxic chemicals. This sharp incline in usage is not just a statistic but a call to action for parents, educators, and policymakers. Vaping products have outpaced regular cigarettes in popularity among adolescents, further complicating prevention efforts. With adolescents exposed to a growing variety of vape liquid flavors and sleek, concealable devices, understanding the scope of teen vaping risks becomes a vital first step for parents wanting to safeguard their children’s future.

What You'll Learn About Teen Vaping Risks
Key facts about teen vaping risks and health effects
How e-cigarette use impacts mental health and nicotine addiction
Strategies for parents to combat teen vaping risks
Frequently asked questions and expert advice
Understanding E-Cigarettes: What Parents Should Know About Teen Vaping Risks
Electronic cigarettes, commonly known as e-cigarettes or vapes, have rapidly evolved and become the most popular tobacco product among young people. Unlike traditional cigarettes, they operate by heating a vape liquid—often flavored and sometimes containing high doses of nicotine—into an aerosol that’s inhaled. Parents may feel overwhelmed by the constantly shifting landscape of vaping products now available to teenagers, from small, USB-shaped pods to disposable devices that can easily be concealed at school. Understanding what e-cigarettes are and why young people are drawn to them is key to addressing teen vaping risks in your household.
Misleading perceptions about e-cigarettes are common among school students, particularly those in middle and high school. Many young people mistakenly believe these products are harmless or just water vapor, when in reality, they can pack a powerful dose of nicotine and other toxic chemicals. These beliefs are reinforced by marketing messages that downplay health risks and position vaping as a “safer” alternative to traditional smoking. Parents should also recognize that accessibility to these products is increasing—often through friends, online stores, or even social media platforms—posing a significant challenge in keeping teens safe from the health effects associated with vaping.
How Do E-Cigarettes Work and What Makes Them Appealing to Young People?
Flavored options targeting young people: Flavored vapes—ranging from candy to fruity blends—are especially popular among youth. Many vaping products are intentionally designed to entice teens, making the risk of early experimentation much higher.
Social media influence and accessibility: Influencers and celebrities often glamorize vaping on platforms frequented by teens, boosting its social status. Vape shops and online retailers also make acquiring products alarmingly simple, sometimes without age verification.
Misconceptions about safety compared to traditional cigarettes: Many students believe e-cigarettes are “safe” because they’re tobacco-free, ignoring the high nicotine content and health risks. This misconception undermines prevention efforts and puts more young people at risk.

Nicotine Addiction and Teen Vaping Risks: The Hidden Dangers
Nicotine addiction is one of the most insidious teen vaping risks, and its impact on young people is especially troubling. The adolescent brain is still developing, making youth far more sensitive to the addictive qualities of nicotine than adults. In fact, studies show that using tobacco products—especially those containing high nicotine concentrations, like certain vape pods—can prime the brain for addiction not just to nicotine, but to other substances in the future. The American Lung Association has repeatedly warned about the unique vulnerability of teenagers, emphasizing how even occasional use can quickly spiral into chronic dependence.
Once ensnared by nicotine addiction, teens may find it increasingly difficult to quit, even if they want to. The withdrawal symptoms—such as irritability, mood swings, difficulty concentrating, and sleep disturbances—are often severe and can disrupt academic, psychological, and social well-being. As electronic cigarette use becomes normalized among peer groups, quitting becomes socially harder, making it vital for parents to recognize early warning signs and intervene promptly. The combination of potent vape liquids, enticing flavors, and targeted advertising continues to draw more young people into a cycle of dependence and risk, escalating public health concerns across the United States.
Why Are Teens Especially Vulnerable to Nicotine Addiction?
Effects on developing brains of young people: Nicotine exposure during adolescence can permanently alter brain development. This can affect memory, learning, attention, and increase the likelihood of lifelong addiction.
Risks of early exposure to nicotine and long-term health effects: Starting nicotine use at a young age exposes teens to greater health risks, including respiratory problems, cardiovascular disease, and negative impacts on mental health due to changes in brain chemistry.
Health Effects of Teen Vaping Risks: What Every Parent Needs to Know
The health effects of vaping go beyond nicotine addiction. Parents need to be aware that even “just vaping” puts teens at risk of harmful exposure to toxic chemicals, heavy metals, and ultrafine particles. These ingredients have been linked to lasting damage to the lungs, heart, and immune system. The U.S. government organizations and American Lung Association warn that what might begin as experimentation can quickly become a chronic habit laden with health risks not yet fully understood due to the newness of electronic cigarette products. This uncertainty only compounds the concern for parents guiding their children through these risks.
Public health experts urge that parents stay vigilant not only about physical health effects but also emerging evidence of mental health repercussions. Studies show strong links between vaping and increased rates of anxiety, depression, and other behavioral issues among adolescents. Recent surges in middle and high school students reporting respiratory symptoms, chronic cough, and hospitalizations due to vaping-related lung injuries solidify that this is not a harmless trend. As we outline below, understanding the specific risks to both body and mind will empower parents to have informed conversations and intervene early to protect their children.
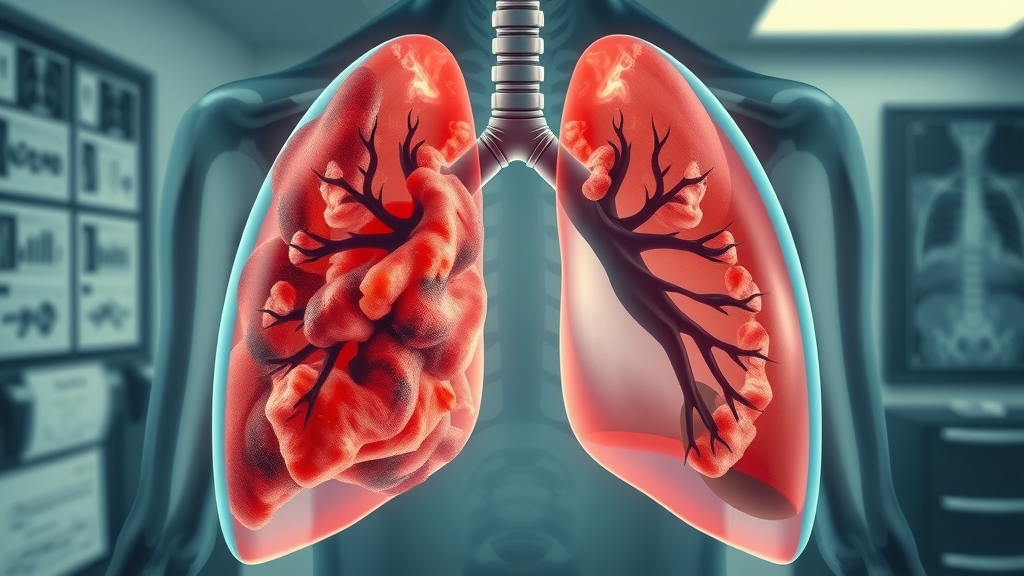
Physical Health Risks: Impact on Lungs and Body
Vaping introduces a variety of harmful substances into the bodies of young people. The inhaled aerosol from e-cigarettes contains not just nicotine, but toxic chemicals, metal particles, and volatile organic compounds—all known or suspected to be harmful according to the American Lung Association. For high school students and middle schoolers, these dangers are magnified because their lungs and other organs are still developing, leading to long-term health effects that can persist well into adulthood. With studies revealing that adolescents who vape are more likely to develop respiratory problems, the risks extend far beyond addiction alone.
Furthermore, vape liquid can harbor heavy metals like lead and nickel, released during the heating process. Public health authorities, including the CDC and American Lung Association, have identified direct links between teen vaping and a heightened risk for severe lung damage, such as EVALI (e-cigarette or vaping-associated lung injury) and other chronic respiratory conditions. The misconception that vaping is simply a safer alternative to smoking regular cigarettes overlooks the accumulation of evidence related to immune suppression, impaired lung function, and susceptibility to infections and illnesses—particularly among young, vulnerable populations.
EVALI and Respiratory Diseases in Young People
EVALI stands for “e-cigarette or vaping associated lung injury”—a condition that has led to thousands of hospitalizations and even deaths among young people in the United States. Symptoms include coughing, shortness of breath, chest pain, nausea, and fever, often progressing rapidly. The CDC reports that while EVALI can affect users of all ages, adolescents are particularly susceptible, given the smaller size and immaturity of their lungs. Studies show that certain contaminants found in vape liquid, especially those in illegal or modified products, exacerbate the risk of severe outcomes, further intensifying teen vaping risks.
In addition to EVALI, young people who vape are at increased risk for chronic respiratory issues, including asthma exacerbation and bronchitis. This is compounded by their developing immune systems, which are less equipped to handle the oxidative stress and inflammation triggered by prolonged e-cigarette use. Parents should also be aware that vaping can worsen pre-existing conditions or create an opening for new respiratory infections, hitting children in middle and high school particularly hard as their bodies struggle to keep up with the onslaught of toxic chemicals and frequent exposure.
Susceptibility to Illness and Immune Suppression
Emerging evidence from leading government organizations in the United States highlights that vaping can weaken the immune defenses of adolescents. Toxic chemicals in vape aerosols—such as formaldehyde, acrolein, and diacetyl—impair the function of cilia in the airways, making it harder for the lungs to clear out bacteria and viruses. This immune suppression not only increases susceptibility to everyday illnesses like the cold or flu but also poses long-term health risks, including chronic bronchitis and even pneumonia.
These health effects are particularly pronounced in young people, who may experience slower recovery times and more severe symptoms. The American Lung Association warns that the cumulative impact of repeated immune suppression from regular e-cigarette use magnifies the risk of ongoing respiratory problems. As middle and high school students continue to experiment with vaping, these hidden dangers should prompt parents to be both vigilant and proactive in discussing risks, recognizing symptoms early, and seeking medical advice when needed.
Comparison of Health Effects: Vaping vs. Traditional Smoking Among Young People |
||
Health Effect |
Vaping (E-Cigarettes) |
Traditional Smoking |
|---|---|---|
Nicotine Addiction |
High; many products contain more nicotine than cigarettes |
High |
Lung Injury (e.g., EVALI) |
Rapid onset of new lung diseases specific to vaping |
Chronic respiratory diseases over time |
Respiratory Symptoms |
Wheezing, coughing, decreased lung capacity even after short-term use |
Wheezing, shortness of breath, chronic bronchitis (long-term use) |
Immune Suppression |
Increased risk of frequent illnesses |
Persistent, but often slower onset |
Long-term Health Risks |
Unknown; early data shows concern for lifelong impacts |
Well-documented risk of cancer, heart disease, stroke |
Mental Health Effects: Teen Vaping Risks Beyond the Physical
Teen vaping risks are not strictly physical; mental health is also at stake. Research from the American Lung Association and major government organizations has revealed strong links between e-cigarette use, anxiety, depression, and behavioral changes among adolescents. Young people who vape are at higher risk for developing mood disorders, and emerging data suggest the substances in vape liquid may alter neurological pathways associated with emotion regulation and reward systems. For school students coping with the pressures of adolescence, vaping can quickly shift from a coping mechanism to a trigger for worsening mental health issues.
Nicotine dependency alone is enough to fuel mental health struggles, as withdrawal can cause irritability, restlessness, and subsequent problems with school performance and family relationships. The cyclical dependency created by regular e-cigarette use makes it even harder for teens to break free, especially if vaping has become normalized within their social circles. Experts warn that the mental health effects of teen vaping risks could linger well after physical symptoms subside, impacting everything from academic progress to self-esteem and social well-being.
Links between vaping and anxiety/depression: Studies show a higher prevalence of anxiety and depressive symptoms among adolescents who vape compared to non-users.
Potential for behavioral and cognitive changes: Long-term use may impact impulse control, attention span, and emotional regulation in developing teenage brains.

People Also Ask: How Harmful is Vaping for Teenagers?
Answer: Teen vaping risks include increased likelihood of nicotine addiction, lung injury, worsened mental health, and long-term health effects that can persist into adulthood.
E-cigarette use among school students exposes them to not only a rapid pathway to nicotine addiction, but also to a complex mix of health risks that are not yet fully understood. The CDC, American Lung Association, and other public health agencies are unanimous: regular use by teenagers can lead to respiratory and cardiovascular issues, mental health changes, inability to focus, and potentially irreversible harm to the developing brain and body. Vaping is never “just harmless fun”—it can leave a legacy of health effects lasting long after adolescence.
People Also Ask: Is it Bad for a 15 Year Old to Vape?
Answer: Yes, vaping at a young age exposes 15-year-olds to substantial health risks, including interference with brain development, risk of lifelong addiction, and increased susceptibility to respiratory illnesses.
Starting to vape as early as age 15 can have dire consequences. This is a critical time for brain development, and exposure to high levels of nicotine can impair learning, memory formation, and emotional health, making it harder for teens to achieve their full academic potential. There’s also a greater risk of establishing a lifelong habit, as well as increased vulnerability to conditions like asthma, bronchitis, and EVALI. These are not theoretical risks—they are increasingly documented in studies from government organizations and the American Lung Association.
People Also Ask: How Does Vaping Affect the Brain of a Teenager?
Answer: Teen vaping risks affecting the brain include impaired cognitive function, memory issues, and heightened vulnerability to addiction, as teenage brains are still developing.
Nicotine exposure during the critical years of brain growth can result in lasting harm. Studies show that vaping can disrupt the normal development of areas responsible for decision-making and impulse control, making it harder for young people to regulate their behavior and emotions. This can set the stage not only for chronic nicotine addiction, but also increase the risks for other types of substance abuse in the future. Parents should be alert for changes in school performance, memory challenges, and pronounced mood swings, which may all be subtle signs of a developing problem.
People Also Ask: What Does Vaping Do to Your Lungs as a Teenager?
Answer: Vaping as a teenager can cause inflammation, lung damage (such as EVALI), chronic coughing, and decreased lung capacity—posing serious health risks.
Teen vaping risks are especially evident in the lungs. Aerosols inhaled from vape liquid can contain ultrafine particles and chemical irritants that reach deep into the delicate tissues of developing respiratory systems. This can result in symptoms like persistent cough, shortness of breath, wheezing, and—in severe cases—acute injuries such as EVALI. Even among young users without preexisting conditions, vaping can decrease lung capacity and make them more susceptible to infections and respiratory diseases. The data is clear: for teenagers, there is no safe level of e-cigarette use.
Why Are Young People Drawn to E-Cigarettes? Understanding Teen Vaping Risks
Peer pressure and social acceptance among young people: Many high school students feel pressured to vape to fit in, especially when they see friends or classmates using e-cigarettes around campus or at social events.
Aggressive marketing strategies by e-cigarette companies: Companies use vibrant ads, influencers, and social media to make vaping look fun, modern, and risk-free — often targeting teens directly.
Influencer and celebrity endorsements: Teenagers are influenced by trends and celebrities promoting vaping, increasing both curiosity and normalization among their age group.

Parental Guidance: How to Talk to Your Children About Teen Vaping Risks
Conversations about teen vaping risks can feel challenging, but they’re crucial for preventing harm. The best defense starts with open, honest, and nonjudgmental communication. Parents should arm themselves with facts, dispel myths their children may have heard at school or online, and create a supportive environment where teens feel comfortable discussing difficult subjects. Highlighting both the short-term and long-term health effects helps teens understand the real stakes without relying on scare tactics. By fostering trust, parents can encourage teens to share their experiences and ask questions before a pattern of use becomes an entrenched habit.
Educational materials from trusted sources, like government organizations or the American Lung Association, can bolster your message. It’s important to remain patient; changing attitudes about vaping may take time, especially when teens face peer pressure, pervasive social media influence, and mixed messaging from advertising. Be prepared to repeat discussions, listen more than you lecture, and seek advice from healthcare professionals if you suspect your child may already be using e-cigarettes. Every parent-child conversation about vaping is a building block toward a healthier, safer future.
Effective Communication Strategies for Parents
Start open, judgment-free conversations: Don’t wait for your teen to ask—initiate the conversation and make it clear you’re a safe person to talk to.
Provide up-to-date facts on health risks: Use resources from official websites and public health organizations to share sensitive information about the realities of vaping.
Encourage questions and honest dialogue: Let your teen know it’s okay to have doubts and to ask questions, even if the subject feels uncomfortable.
Seek professional help when necessary: If you notice warning signs of nicotine addiction or deteriorating mental health, consult a healthcare provider for expert guidance and intervention.
Key Takeaways: Protecting Your Teen from Vaping Risks
Stay informed on the latest data and health effects: Knowledge is power. Reliable, updated information helps you guide your child effectively.
Recognize signs of vaping and nicotine addiction: Watch for physical symptoms, behavior changes, and clues like unusual devices or scents.
Support mental health and create a safe environment: A strong support system can make it easier for teens to resist peer pressure and recover if they’ve already started vaping.

Expert Quotes on Teen Vaping Risks and Health Effects
"Teen vaping risks extend far beyond addiction; they shape the health and futures of an entire generation." – Dr. Amanda Reynolds, Pediatric Pulmonologist
Frequently Asked Questions (FAQs): Teen Vaping Risks
What chemicals are present in e-cigarettes?
E-cigarette vapor often contains nicotine, flavorings, heavy metals (like lead and nickel), formaldehyde, and other toxic chemicals. These ingredients can cause lung damage, impact the developing brain, and even increase cancer risk.Can quitting vaping reverse health effects in young people?
Many health effects from vaping—especially in the early stages—can improve once a teen quits. Lung function and mood may gradually return to normal. However, some damage, especially with long-term use, may be lasting. Early intervention increases the likelihood of a full recovery.How can schools address rising teen vaping risks?
Schools play a critical role by implementing clear policies, offering education about health risks, providing support groups, and collaborating with local health organizations. Early education and a strong partnership between home and school are vital to prevention.
Conclusion: Taking Action Against Teen Vaping Risks
Why Parental Awareness and Advocacy Matter
Parents have a pivotal role in shaping attitudes and behaviors around vaping. By staying vigilant, informed, and proactive, you can help protect your teen's health and future from the escalating risks of e-cigarette use. Open dialogue and ongoing education will make a world of difference.
Resources for Parents and Guardians Seeking Support
If you’re concerned, turn to reputable organizations such as the American Lung Association, local school counselors, health care providers, and official government websites. They offer trustworthy information, support, and actionable steps for prevention and recovery.
CTA: Stay Informed and Proactive About Teen Vaping Risks
Stay connected, stay informed, and remain proactive—your actions today can help protect your teen for years to come. For more tips and resources on navigating teen vaping risks, visit nationwide health organizations or talk to your family doctor.
 Add Row
Add Row  Add
Add 





Write A Comment